One of the most prevalent public health issues, diabetes affects 387 million people worldwide, with type 2 diabetes accounting for over 90% of cases (DM type 2) [1]. Diabetes, which is currently the fourth most common cause of death and illness globally, is on the rise. It is imperative to attain optimal glycemic control at an early stage in order to avert complications and death [2]. Despite the fact that only 53.6% of type 2 diabetics reach the desired goal of a glycated hemoglobin (HbA1c) of less than 7% [3]. Personalized targets are recommended by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) based on a number of factors, including co-morbidities, patient preferences, needs, values, duration of diabetes, risk of hypoglycemia, costs, and the assurance of a patient-centered approach [4]. Targets of less than 6.5% for newly diagnosed patients and less than 7.5% for people receiving two or more medications are advised by the National Institute for Health and Clinical Excellence (NICE) in the United Kingdom [5]. One of the main causes of not reaching these goals is the co-occurrence of psychological problems.
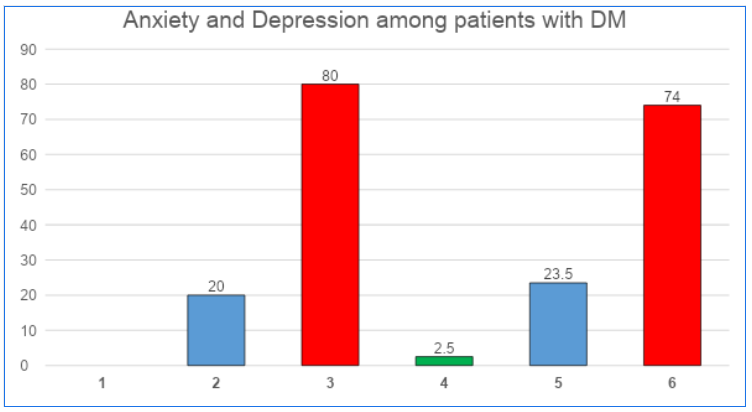
Roughly 10–20% of elderly people experienced symptoms of depression [6]. The risk is higher—between 25 and 33 percent—for people with chronic diseases [7]. According to Yaseen and Dauod (2019) [8], these illnesses have a detrimental impact on quality of life and have significant economical ramifications [9]. According to several studies (Lustman et al., 2000; Gross et al., 2005) [10-11], diabetes patients have a higher prevalence of depression, which contributes to their poor glycemic control and complications. According to other research, depression is linked to both cognitive decline and physical disability, both of which are more common in people with diabetes [12-13]. And additionally imply that depression frequently has a prolonged course [14-15]. Depression and anxiety symptoms may arise as a result of the neuroendocrine abnormalities linked to diabetes mellitus (DM), such as elevated cortisol levels and changed dopamine concentrations [16-17]. The purpose of this research is to identify diabetes patients' levels of anxiety and despair. To ascertain the association between diabetes patients' anxiety and depression and demographic information like age, gender, etc.
The International Diabetes Federation estimates that one in eleven persons worldwide suffers from diabetes, and that one in fifteen adults worldwide has impaired glucose tolerance. These statistics support the organization's claim that diabetes is "one of the largest global health emergencies of the 21st century." It is projected that these numbers will rise sharply, especially among urban residents, leading to an increase in medical and financial problems [18]. It is anticipated that this increase will bring the total amount spent on diabetes treatment to 12%. In Iraq, the total number of people affected by diabetes was 561000 in 1995 and 678000 in 2000; by 2025, that figure is predicted to rise to 1,739,000 [19]. According to Bromet et al. (2011) [20], the lifetime prevalence of depression, a highly serious illness, ranges from 11% in low-income nations to 15% in high-income ones. According to Hewlett et al. (2014) [21], there is a 50% lifetime risk of mental health issues, along with a significant decline in productivity and employment. In high-income countries, diabetes is thought to be the eighth cause of disability-adjusted life years, while depression and anxiety rank fourth [22]. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) published by the American Psychiatric Association defines depression as a mood disorder that reunites multiple symptoms that impair an individual's functionality. Emotions, thoughts, and actions are disrupted by depression [23]. Depression is classified as a first episode, a recurrent or chronic episode, mild, moderate, or severe, with or without psychotic symptoms, according to the DSM-5. Research has demonstrated that there is a higher chance of depression in individuals with pre-diabetes and diabetes who are not yet diagnosed. Diabetes is more common in patients with a history of the illness than in healthy individuals. and could be two times higher in type 2 diabetics than in the general population [24].
Anxiety and depression can exacerbate the prognosis of diabetes, increase medication non-adherence 9, and lower health-related quality of life. Additionally, there is a risk of According to Rubin et al. (2008) [25], the risk of type 2 diabetes mellitus increases to 60%. There seems to be a reciprocal, intricate interaction between depression and diabetes. biological mechanisms, the understanding of which improves harmful consequences. Recent assessments of the literature have indicated three possible routes for the relationships. Diabetes may increase the likelihood of depression in the future, and depression may have a common etiology with diabetes. This cross-sectional study sought to highlight the need of screening for depression in individuals with diabetes and to demonstrate the connections between depression and diabetes [26].