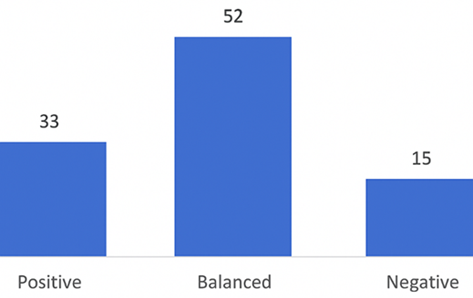
The primary findings of this audit demonstrated a significant deviation from established preoperative fasting guidelines, with only 26.6% of patients adhering to the recommended 6-8-hour fasting period.
The minimum, maximum, and mean fasting hours in an study by Gebremedhn and Nagaratnam in 2014 were 5, 19, and 12.72, respectively [6]. More than 95 % of their patients fasted from fluid longer than the recommended preoperative fasting times of the ASA [5]. Prolonged fasting hours have also been noted by other studies as well [8,9].
Despite the latest guidelines recommending shorter fasting periods, our audit revealed an average fasting span of 9.8 hours, with 44.9% of participants fasting over 10 hours. This indicates a significant lapse from our hospital’s preoperative fasting guideline that conforms to the ASA standard guideline [5].
We noted that surgeries scheduled in the afternoon were associated with longer fasting times compared to surgical procedures planned for morning surgeries. The age group of 60-80 years exhibited the longest average fasting durations.
Similar findings were reported in the BIGFAST study, encompassing 3715 patients [10], and a study [11], both highlighting prolonged fasting durations despite the adoption of ERAS protocols. The BIGFAST study noted a significant difference in median fasting times between traditional and modern fasting protocols.
Furthermore, a 2023 update by the American Society of Anesthesiologists endorsed guidelines allowing clear liquids up to 2 hours preoperatively for healthy adults. However, our study and others displayed that even institutions following updated fasting protocols still record average fasting times exceeding recommendations, emphasizing real-world challenges in guideline implementation.
Studies exploring pediatric populations also indicated variations in fasting practices. An update from the European Society of Anaesthesiology recommended reduced fasting durations for clear caloric solutions in pediatric patients, emphasizing positive patient outcomes and the potential role of ultrasound in assessing gastric contents.
In conclusion, despite evolving guidelines advocating for shorter fasting periods, our study alongside similar studies revealed persistent challenges in translating these guidelines into routine practice. Factors contributing to prolonged fasting include afternoon surgeries, unpredictable schedules, patient diversity, and communication gaps among healthcare professionals. Further research is needed to understand the underlying causes of prolonged fasting and to develop strategies for effective guideline adherence.
There is a pressing need for healthcare professionals to enhance their familiarity with contemporary fasting guidelines and prioritize comprehensive education for both patients and the healthcare team. Future research initiatives should focus on developing effective strategies to address prolonged fasting instances.