Patients
An elective cesarean section was included in 60 pregnant women with ASA I-II status who were 18 years and older. Case reports, fetal anomaly, fetal growth retardation, Rh incompatibility, and congenital malformations such as obstetric complications and cases less than 2500 grams of the fetus were excluded from the study.
Study Protocol
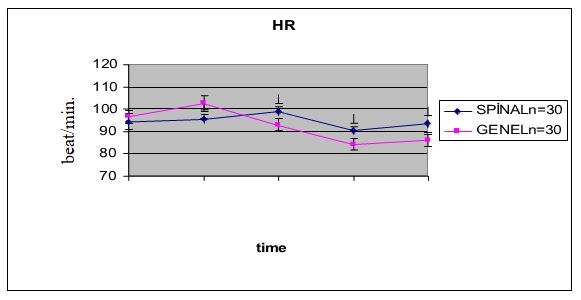
The study was carried out with the approval of the Ethics Committee of Meram Medical Faculty of the University of Selcuk (2011/017 dated 27.01.2011). All patients were informed about the preoperative operation, and their approvals were obtained. Patients were randomly divided into two groups general anesthesia and spinal anesthesia. A computer-generated randomization program using a random block size was used. After all, patients were taken to the operation room, IV injection was performed with an 18 G cannula, and 10 ml/kg isotonic was given, and they were kept in a 15 ° left lateral tilt position until the end of the operation. In both groups, 100% O2 and 3-5 minutes of preoxygenation were applied to the cases. The age, height, weight, and gestational week of each patient were recorded in the operation room. Systolic arterial pressure (SAD), diastolic arterial pressure (DAB), mean arterial pressure (MAP), peripheral oxygen saturation (SpO2), and heart rate (HR) were measured, and the values were recorded as baseline values. The same measurements were recorded after intubation in the general anesthesia group, 5 minutes after the operation started, and repeated every 5 minutes until the end of the operation. 10IU oxytocin was slowly given IV in both groups. 10-20 units of oxytocin were added into 1000 ml of isotonic.
The 1st and 5th min APGAR values of the newborns were evaluated by the same pediatrician. Umbilical artery blood gas 2nd-hour and 24th-hour NACS values of all newborns were recorded. In both groups, the onset of anesthesia-infant hatching, uterine incision, infant hatching, and anesthesia duration, resuscitation requirement of the newborn ( mask ventilation or intubation) were recorded.
The patients in the Spinal Anesthesia group were recorded 5 minutes after the operation was started and every 5 minutes at the end of the operation. After the skin disinfection with the appropriate antiseptic solution was provided to all pregnant women, a 25 G atraumatic spinal needle from the L3-L4 interval was entered into the subarachnoid space. Bupivacaine 10mg was given after the free, clear CSF flow. In the case of significant hypotension in the spinal anesthesia group (starting from 20-30% of the initial SOD), ephedrine 5-10 mg IV bolus was performed. 20 mg IV tenoxicam was administered to the spinal anesthesia group after the delivery of the baby for postoperative analgesia.
In the general anesthesia group, a dose of 0.5 μg/kg remifentanil was given as a bolus in 30 sec and then infused at 0.2 μg/kg/min. İntravenously. The induction was completed with 1.5 mg/kg thiopental and 1 mg/kg succinylcholine. Endotracheal intubation was performed after muscle relaxation. Anesthesia was maintained with remifentanil infusion (0.2 μg/kg/min) at 50% O2 + 50% N2O. At the end of the operation, remifentanil infusion was closed when the fascia was closed, N2O was closed, and 100% O2 was given. In order to provide postoperative analgesia, 2 mg/kg tramadol and a 20 mg IV bolus of tenoxicam were administered to the general anesthesia group.
When there was a sign of wakefulness in the general anesthesia group (eye-opening, eye wrinkling, hand-foot motor response) or SAB increased by 25% compared to baseline, remifentanil dose was increased by 25%; The remifentanil dose was reduced by 25% when SAB was 25% below baseline or below 90 mmHg. The reduction of HR to less than 50 per minute was accepted as bradycardia, and a bolus of atropine 0.5 mg was planned.
In both groups, the onset of anesthesia, infant hatching, uterine incision, infant hatching, and anesthesia duration, resuscitation requirement of the newborn ( mask ventilation or intubation) were recorded. In the postoperative period, the first time that the newborn could effectively receive the mother's breast was recorded as sucking time. All neonates were monitored by a pediatrician for 30 min after cesarean section. In terms of side effects that may develop in the newborn, physical conditions, masking devices, and all kinds of resuscitation equipment were made available for mask ventilation and endotracheal intubation.
Statistical Analysis
SPSS 22 (IBM, Armonk, NY) version was used for statistical analysis. In the case of the normal distribution of quantitative data, it is compared with the Student's t-test. Otherwise, the Mann-Whitney U test was used. Qualitative data were compared with Pearson's chi-square test. A p-value of less than 0.05 was considered statistically significant.