Laparoscopic procedures are widely accepted in the clinical practice, now-a-days with various advantages as compared to open procedures. But, laparoscopy procedures are also associated some disadvantages like greater alteration in hemodynamic parameters intraoperatively, primarily due to extra peritoneal or intraperitoneal CO2 insufflation to achieve pneumoperitoneum and secondarily due to position given in some laparoscopic procedures, So, the drugs given during laparoscopic procedures should be such that it should not compromise the advantage of laparoscopy and at the same time minimizes hemodynamic changes due to CO2 insufflation.
Clonidine is an imidazoline derivative that acts as an alpha 2 agonist. It has analgesic properties and induces preoperative anxiolysis and sedation. clonidine not only has potential to attenuate sympathoadreanl response to laryngoscopy and tracheal intubation but it also improves the intraoperative hemodynamic stability along with reduction in the intraoperative requirement of anaesthetic agents and postoperative pain. [2] Clonidine inhibits release of catecholamine’s and vasopressin and thus modulates hemodynamic changes associated with pneumoperitoneum. [38]
Magnesium inhibits catecholamine release from both the adrenal gland and adrenergic nerve terminals . By acting as an antagonist of N-methyl d-aspartate (NMDA) receptors, magnesium (Mg) has the potential to treat and prevent pain. [4–5] Mg suppressed NMDA-induced adverse behavioural reactions and hypersensitivities caused by nerve injuries in animals. Magnesium's role in reducing analgesic requirements during the postoperative period was demonstrated in a clinical study.[6] Magnesium administration, according to Koinig et al [15], resulted in a significant reduction in fentanyl consumption during the perioperative period. Intravenous magnesium sulphate reduces catecholamine release during tracheal intubation. It also has direct action on blood vessels causing vasodilation and at higher doses, it reduces vasopressin-mediated vasoconstriction.
Various studies have been carried out to find out efficacy of clonidine and magnesium sulphate as adjunct to general anaesthesia in providing intraoperative hemodynamic stability and decreased anaesthetic consumption like Kodaka M. et al 13, Imai Y et al 16, Fehr S.B. et al 8, Telci L. et al 9, Altan A. et al 10, Ray M. et al 30 and the results of these studies are quite favourable.
In this study group, clonidine was used in doses of 3 mcg/kg of body weight this dose was used considering its favourable results as per study of Altan and Turgut et al 10 in 2005 they used clonidine 3 mcg/kg in 20 ml saline intravenously over a period of 15 minutes before induction and 2mcg/kg /hour by continuous infusion intraoperatively, in their study, they found significant rates of bradycardia and hypotension. 4.5 mcg/kg clonidine significantly reduced mean arterial pressure prior to anaesthesia induction, according to Aho M. et al 40. As a result, they advised 3 mcg/kg of clonidine for perioperative hemodynamic stability. Based on these findings, we gave clonidine 3 mcg/kg intravenously 15 minutes before induction and did not use continuous infusion intraoperatively.
Seyhan T.O. et al 11 2006 used 40mg/kg magnesium sulphate as bolus before induction followed by infusion at 10mg/kg/hr or 20mg/kg/hr for next 4 hours they observed that increasing magnesium doses did not offer advantages intraoperatively, but rather induced hemodynamic consequences, Elsharnouby N.M. et al 41 used magnesium sulphate 40mg/kg intravenously over a period of 15 minutes before induction and 15mg/kg/hr by continuous infusion intraoperatively they noticed more episodes of severe hypotension using this dose of magnesium sulphate taking into consideration the results of the above mentioned studies in our study we only used a single bolus dose of magnesium sulphate 40mg/kg before induction and we did not used any magnesium infusion intraoperatively the dose selected by resulted in a steady and smooth reduction of blood pressure and heart rate.
After study drug infusion patients were premedicated with inj. glycopyrrolate 4μg/kg IV as routine anticholinergic premedication to protect from vagal reflexes and as antisialogue and inj. fentanyl citrate 2mcg/kg of body weight IV 10 min. before induction. Propofol was used as inducing agent in all three groups, time for BIS to decrease more than 60 noted as induction period.[10] The mean induction period was significantly less in Group M and C, The overall mean requirement of Propofol dose for induction was significantly less in magnesium sulphate and clonidine group (p<0.001) compare to control group. Similar findings were observed by Richards M.J. et al 7, Goyagi T. et al 17 , Marinangeli F. et al 19, Fehr S.B.et al 8, Altan A. et al 2005 10, Paris A. et al 29, and Ray M. et al. 30, The reduced induction dose of propofol in clonidine pretreated group can be considered as an additive hypnotic effect of clonidine.
The overall mean requirement of Propofol infusion for maintenance was significantly less (p<0.001) in magnesium sulphate and clonidine group compare to control group Our findings were similar to, Fehr S.B. et al 8, Telci L. et al 9, Morris J. et al 24, Altan A.et al 10, Seyhan T.O.et al 11, Ryu J.H.et al 27, Ray M. et al30.
In our study, propofol requirements were significantly lower in both Group C and Group M compared to Group S. Kulka P.J. et al 42 reported that studies with rat model showed, at clinical concentration clonidine partially inhibits voltage-gated Na+ and K+ channels and suppresses the generation of action potentials in tonic firing spinal dorsal horn neurons. This may contribute to the reduction of propofol and fentanyl requirements. [30]
James M.F. et al 3 stated that MgSO4 has been reported to produce general anaesthesia and enhance the activity of local anaesthetic agents. Depressant effects of MgSO4 on the central nervous system (CNS) of animals have been reported too.[4] Woolf C.J. et al 5 stated that magnesium antagonized NMDA receptors in the CNS. Another mechanism could be that magnesium decreases peripheral nociceptor sensitisation or the stress response to surgery by reducing catecholamine release via sympathetic stimulation. However, these mechanisms do not explain the decrease in propofol requirements, so more research on the interaction of magnesium and propofol as sole agents is needed. By acting as an antagonist of NMDA receptors, magnesium has the potential to prevent pain.[5] Koinig H. et al 15 first evaluated the effect of magnesium on perioperative analgesic requirement in patients with identical level of surgical stimulation. Shulz-Stubher et al.43 also confirmed this in their study.
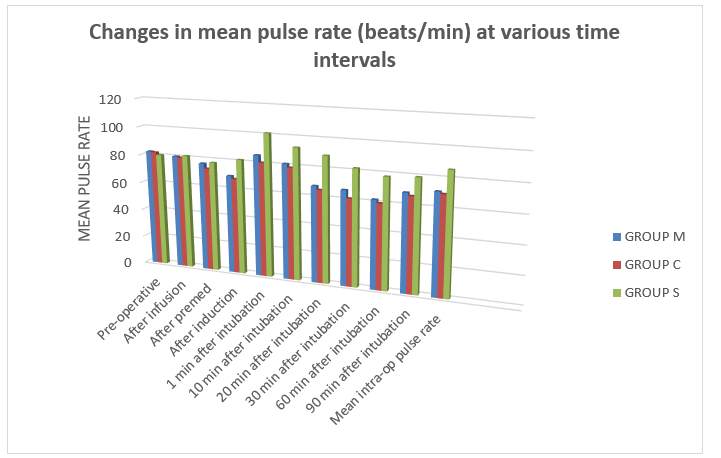
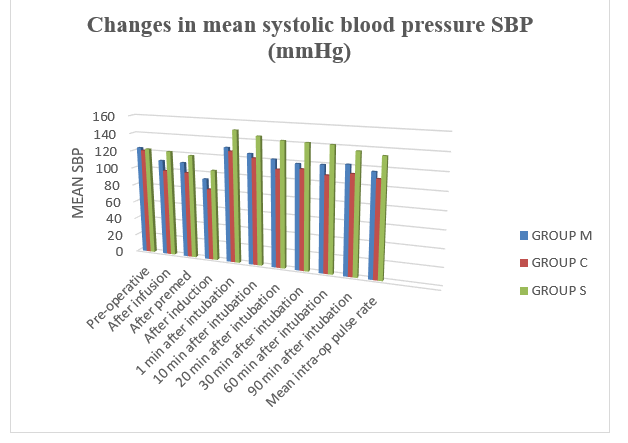
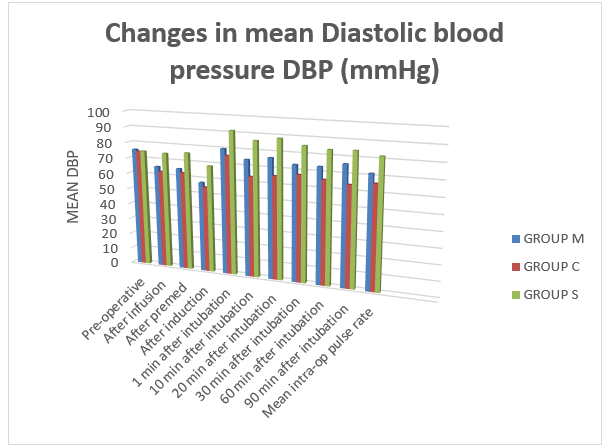
Laryngoscopy and intubation is considered to be stress response and increase in pulse rate, systolic blood pressure and diastolic blood pressure is expected during these events. Pre-treatment with magnesium sulphate and clonidine provided better protection against sympathetic stimulation due to laryngoscopy and intubation and leading to blunting of intubation response. Kodaka M. et al 13, Imai Y. et al 16, Altan A. et al 10, Seyhan T.O. et al 11, Ray M. et al 30 and Das M. et al. [44].
After co2 insufflation there was increase in pulse rate in all three groups but it was significantly increased more in control group (Group S) rise in pulse rate was due to activation of sympathoadrenal or humoral response but pulse remained on stable side in group M and group C due to pre-treatment with magnesium sulphate and clonidine which lead to attenuation of the hemodynamic response to pneumoperitoneum. Kalra N.K. et al 31, Das M. et al 44, Singh S. et al.45
Pulse remain stable and on lower side in group M & C throughout intraoperative period whereas it was on higher side in control group there was significant difference among the three groups (p<0.05), suggesting that Clonidine and magnesium lead to hemodynamic stability intraoperatively. Altan A. et al 10, Ray M. et al 30, Kalra N.K. et al 31, Das M. et al 44, Singh S. et al.45
Preoperative premedication with magnesium sulphate and clonidine lead to stable hemodynamic after intubation. [19,10,11,30,45]
Fehr S.B. et al 8 reported that clonidine administration resulted in a lower propofol requirement for certain level of anaesthesia to be achieved as defined by similar BIS values. The fact that no explicit intraoperative awareness occurred and no signs of implicit memory were observed indicates that the anaesthetic state induced by a clonidine and low dose propofol may be similar to the anaesthetic state induced by a larger dose of propofol alone. It is evident that larger trials will be necessary to show conclusively that lower dose of propofol combined with clonidine is as safe as a larger dose of propofol in preventing intraoperative awareness. Lee D.H. et al 46 stated that, recent studies have demonstrated that magnesium administration significantly reduces anaesthetic drug requirements and attenuation of BIS increases, suggesting that magnesium sulphate may have a sedative effect and thus might be beneficial.
Hence, in our study titrating propofol infusion rate with BIS monitoring during balanced anaesthesia decreased propofol use and significantly improved recovery in our study. These findings indicate that the use of BIS may be valuable in guiding the administration of propofol intraoperatively. Gan T.J. et al 14, Fehr S.B. et al 8, Altan A. et al 10, Seyhan T.O. et al11, and Ray M. et al.3
Time for BIS to rose up to 80 after stoppage of propofol infusion was recorded as recovery time in each group as per Altan A. et al.[10]The mean recovery time was found to be 9.23 ± 2.45 min in group M, 6.86 ± 1.56 min in group C and 7.36 ± 2.05 min in group S. It was significantly prolonged in magnesium group (p<0.001). Mean recovery time was comparable in group C and group S (p>0.05). Similar findings were observed by Altan A. et al 10, Ray M. et al.30
Extubation time was calculated from stoppage of propofol infusion stopped till the tracheal extubation of patient after ensuring adequate reversal, sustained (>5sec) head lift and a forceful hand grip.We observed that recovery time was faster in clonidine and was prolonged in magnesium group due to central depressant effect of magnesium sulphate.
Richards M.J. et al 7 found significant delay in recovery in clonidine premedicated patients due to the use of high dose of clonidine (8.5μg/kg) in combination with a benzodiazepine. Guglielminotti J. et al 2 with the 5μg/kg dose of oral clonidine failed to detect any delay in recovery from patients leading to early extubation compare to magnesium and control group. This was also consistent with the data of Kumar A. et al 47 and Ghingone M. et al 48, who have reported a faster recovery in elderly patients undergoing intraocular surgery and premedicated with 5μg/kg clonidine when compare with patients premedicated with diazepam.
Magnesium group was associated with delayed recovery this could be due to central depressant action of magnesium sulphate. Guglielminotti J et al 2, Altan A. et al 10, Seyhan T.O. et al 11, Ray M. et al 30and Kalra N.K. et al.31
When the groups were compared for the parameters of recovery; response to verbal commands and orientation time as per Altan A. et al 10 we found that these parameters were longer with group M (P<0.001) there were no significant difference between other two groups (P>0.05) this delay in recovery in magnesium group may be due to CNS depressant effect of magnesium sulphate. Peck C.H. et al 49 in their study attempted anaesthesia by magnesium sulphate infusion in three patients of herniorrhaphy and reported a narcotic state. However, Aldrete J.A. 50et al suggested that this was actually a sleep like state caused by cerebral hypoxia from progressive respiratory and cardiac depression. When ventilation was maintained even very high level of serum Mg produced no central nervous system depression. Kalra N.K. et al 31 stated that magnesium sulphate potentiates neuromuscular blockade induced by non-depolarizing neuromuscular agents and this possible was the cause of prolongation in recovery. Patient in clonidine group had early recovery except for delayed orientation time this could be due to known sedative action of clonidine. Telci L. et al 9, Altan A. et al 10, Seyhan T.O. et al 11, Ray M. et al 30, and Karla N.K. et al.31
The mean pain score in the immediate post-op period was found to be lower in group M and group C compared to group S which was statistically significant (p<0.001). Noxious stimulation leads to the release of neurotransmitters, which bind to various subclasses of excitatory amino acid receptors, including NMDA receptors. Activation of these receptors leads to calcium entry into the cell and initiates a series of central sensitization such as wind-up and long term potentiating in the spinal cord in the response of cells to prolonged stimuli.[52] Woolf C.J. et al 5 stated that NMDA receptor signaling may be important in determining the duration of acute pain. Magnesium blocks calcium influx and noncompetitively antagonizes NMDA receptor channels. [53] Non-competitive NMDA receptor antagonists can have an effect on pain when used alone. [54] As magnesium sulphate has NMDA receptor antagonist action this may lead to postoperative pain relief in magnesium pre-treated group. Clonidine induces dose-dependent spinal cord antinociception, mainly through stimulation of α2-adrenoceptors in the dorsal horn, mimicking the activation of descending inhibitory pathways.[55]Koining H. et al 15, Seyhan T.O. et al 11, Ryu J.H. et al 27, Tramer M.R. et al.6
Wadhwa et al [56] suggested that magnesium sulphate infusion reduces the shivering threshold in humans, and IV magnesium sulphate has been reported previously to suppress post- anaesthetic shivering.[57] Shivering causes discomfort and aggravates postoperative pain [58 ] and the prevention of shivering may attenuate postoperative pain and enhance patient’s satisfaction.
PONV was a common side effect observed in all the groups in the recovery room. Mikawa et al 59 and Handa et al 60 have reported a reduced incidence of PONV after premedication with clonidine in children undergoing strabismus surgery and Oddby M.E. et al 61also reported antiemetic effect of clonidine after breast surgery in adults. Singh S. et al 45 in their study reported decreased Incidence of nausea and vomiting in clonidine group compare to control group (28% Vs 52%).
A general reduction in sympathetic outflow caused by clonidine [62], could also attributed to the reduction of PONV, since a high sympathetic tone and catecholamine release may trigger nausea and vomiting.[63,64] Further studies are necessary to gain better understanding regarding which of the afore-mentioned mechanisms that is most important with regard to the antiemetic effects of clonidine.
Delayed recovery associated with magnesium due to its CNS depressant action also the potent sedative activity of clonidine is associated with greater degree of sedation and drowsiness in post-operative period. Telci L. et al 9, Altan A. et al 10, Seyhan T.O. et al 11, Ray M. et al 30, and Karla N.K. et al.31
It was thus observed that pre-treatment with magnesium sulphate and clonidine lead to better obtundation of pressor response and also provided optimum hemodynamic stability throughout the laparoscopic surgical procedure and also reduced propofol consumption for induction as well as for maintenance. Both clonidine and magnesium sulphate caused bradycardia and hypotension and magnesium sulphate caused delay in recovery. Therefore, both clonidine and magnesium sulphate need careful management, to be used as adjuvant agents to general anaesthesia.